The Healthcare Hub
Compliance and Credentialing: Does an Open-Door Policy Leave Your Organization at Risk?
-
 Jennifer Williams, GHX Director of Market Development & Education, Credentialing
Jennifer Williams, GHX Director of Market Development & Education, Credentialing
Until recently, almost anyone could enter a hospital or physician’s office with relative ease. Facilities were designed to allow access. Today, while many professional office buildings require check-in and access badges, countless healthcare facilities have not adopted safety protocols to this degree. But that’s changing and for good reason.
Physical access is just one of the many processes of healthcare facility management that have come under scrutiny as a result of the 1999 To Err is Human report, which asserted that the challenge isn’t bad people in healthcare, but good people working in bad systems that need to be made safer.1
Building best practices into the system
As To Err is Human1 and subsequent studies point out, a comprehensive compliance program can improve the safety and security of patients and staff by making it easier for business visitors to follow best practices and system policies.
A strong compliance program can assist facilities in the prevention of adverse events like healthcare-associated infections (HAIs), falls, violent crimes, and theft. And while there are certain costs associated with staffing a compliance program, the human, financial, legal, and regulatory costs of NOT fielding a comprehensive compliance initiative can be significantly higher.
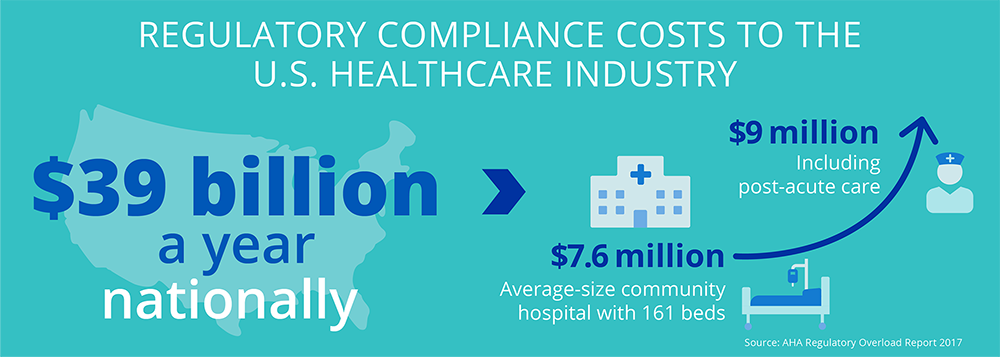
$39 billion: That’s how much it costs the U.S. healthcare industry each year to manage regulatory compliance, according to the American Hospital Association.2 Breaking it down further, an average-size community hospital with 161 beds could be spending as much as $7.6 million annually — and up to $9 million if they have post-acute care.3
The evidence for more robust compliance models, vendor risk models, and credentialing systems in healthcare is indisputable — first and foremost for patient and staff safety, but also for quality improvement and cost control.
Facing the challenges of a rapidly changing environment
With compliance models still evolving in response to regulatory requirements (at the time of this writing, 629+ discrete ones across the nine major domains), COVID-19 and more, there’s little standardization or consistency from one healthcare facility to the next. This is especially true since the "COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers" were issued in March 2020, which have temporarily4 suspended, relaxed or postponed a wide range of federal regulations.
As providers struggle to develop and implement policies and procedures based on rapidly evolving compliance best practices and regulatory requirements, they find themselves running on limited data — and even more limited insights into the essentials of a successful compliance program.
On the other hand, vendors are experiencing increased friction at a time when the facility entry process has already become incrementally more difficult. As procedures and requirements continue to vary dramatically from one healthcare facility to another, they find themselves wrestling with rising administrative loads while attempting to return to normalcy. It’s difficult to know what to expect from one facility to another, so each encounter with a new or developing vendor access program can feel like yet another obstacle.
So, what’s the answer? Expert guidance makes credentialing work better for providers and suppliers
Solutions and procedures need to allow for:
- System-wide policy standardization, and
- Easy, fast, and safe facility access
While it will take time for healthcare facilities to standardize credentialing procedures, (and differences are likely to remain) insights into the performance of various measures can accelerate the process. Healthcare systems need technology partners with expertise in the challenges, vulnerabilities, and best practices of compliance-specific healthcare matters.
GHX Vendormate offers credentialing insights that can help facilities avoid recreating the wheel when it comes to vendor access. We’ve developed a five-part framework that facilities can use to improve compliance across every level of the organization. Our team of professionals can help identify potential compliance gaps and will make recommendations on best practices to support your organization’s goals.
Our automated vendor monitoring capabilities and real-time reports help identify issues and sanctions that mitigate risk for a health system. Meanwhile, our mobile app and touchless kiosk support fast, safe, contact-free check-in for vendors and visitors. These solutions scale easily, allowing for standardization and consistency across an entire IDN.
In addition, GHX Vendormate has just announced the expansion of our world-class vendor credentialing digital solution to include non-business visitors. Our research indicated that organizations preferred the ability to manage both vendor and visitor badging using the same platform. Based on this feedback, our development team has made both options available with a simple software upgrade.
Working with health systems on a daily basis, my team of Compliance Solution Specialists and I have become all too familiar with the gaps that are often overlooked or missed. We recommend a review of potential issues and stand ready to assist in assessing your compliance program and identifying opportunities for improvement.
Schedule a Complimentary Compliance Review
1Institute of Medicine (US) Committee on Quality of Health Care in America, To Err is Human: Building a Safer Health System, 2000.
2American Hospital Association, Regulatory Overload: Assessing the Regulatory Burden on Health Systems, Hospitals and Post-Acute Care Providers, October 2017
3HealthcareSource, “Understanding the True Costs of Healthcare Regulatory Compliance,” accessed July 2021
4 PYA, “Compliance During and After COVID-19,” April 28, 2020
5 The Health Law Firm, 2021
6 ProviderTrust, 2015
